Unfortunately, glaucoma damage is permanent. Once you’ve been assigned a glaucoma diagnosis, your eye doctors able to treat you with eye drops that can either decrease your eye fluid production or help to open up the drainage area in your eye. Your only other option is surgery. You should discuss all of your treatment options with your local eye doctor or with our optometrist in New York City Dr. Saba Khodadadian or ophthalmologist Dr. Richard L. Deluca in detail. Get the eye care you need in the safe, reassuring hands of the best in class eye doctors in NYC.
Glaucoma
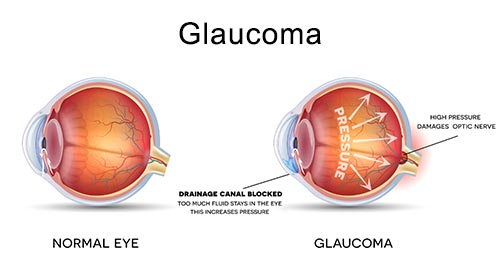 Glaucoma is actually a term that covers a group of diseases that lead to loss of vision, typically through subtle changes in your eye pressure over time. The pressure is changed by a buildup of fluids in the front part of your eye. Glaucoma occurs when the balance of fluids entering and leaving your eye is disrupted, and the flow of fluids out of the eye doesn’t happen the way it should.
Glaucoma is actually a term that covers a group of diseases that lead to loss of vision, typically through subtle changes in your eye pressure over time. The pressure is changed by a buildup of fluids in the front part of your eye. Glaucoma occurs when the balance of fluids entering and leaving your eye is disrupted, and the flow of fluids out of the eye doesn’t happen the way it should.
The resulting high eye pressure damages your optic nerve, which can lead to irreversible vision loss or even total blindness. If it’s caught in time, medications can restore your eye pressure and halt the progression of the second-leading cause of blindness in the U.S.
Symptoms over Time
Glaucoma is a slow-progressing disease that doesn’t usually have symptoms. There are several types of glaucoma, so symptoms can vary, depending on the type. If you’re among the 50 percent of people who have glaucoma symptoms, you may experience one or more of the following:
- Blind spots in your peripheral vision
- Blurred vision
- Halos around lights
- Headaches
- Eye pain
If you are having any visual abnormalities you should always be evaluated with a thorough consultation and examination by a physician for an accurate diagnosis and treatment plan as it may be a symptom or sign of a serious illness or condition.
Main Causes of Glaucoma
It’s not unusual for there to be no concrete reason for your glaucoma. A popular theory is that the blood supply to eye is not at a normal level. Whatever the cause, the drain opening in your eye either closes or becomes clogged. Only secondary glaucoma has definite causes, such as a tumor or diabetes.
Glaucoma has been found to run in families, so if someone in your family has already been diagnosed with glaucoma, be sure to inform your eye doctor so that your eye pressure can be tracked too. Everyone’s normal eye pressure is different, and it even varies from day to day and from hour to hour, depending on your activities and environment. Get your pressure checked regularly to establish an average eye pressure that’s normal for you.
Tests Can Vary
The test most people are familiar with is the “puff test,” which is a basic glaucoma screening test to estimate your eye pressure. The normal range of pressure is 12 to 22 millimeters of mercury (or mmHg). However, as previously mentioned, eye pressure is unique to each patient. If your results don’t fall within what is considered a normal range, then your ophthalmologist or New York optometrist more than likely moves on to other glaucoma tests to fully evaluate the health and functioning of your optic nerve, as well as to get a more accurate pressure reading. Other tests include:
- Tonometry, which measures inner eye pressure using eye numbing drops
- Ophthalmoscopy, a dilated-eye exam that looks at the shape and color of your optic nerve
- Perimetry, a visual field test that checks your complete field of vision
- Gonioscopy, which examines the angle in your eye where the iris and the cornea meet
- Pachymetry, which measures the thickness of your cornea
Many Types of Glaucoma
- Primary open-angle glaucoma is the most common form of the disease. A slow-progressing and painless disease, you may not know you’re even experiencing an eye problem until you see large spots or begin to experience other loss of vision indicators.
- Normal-tension glaucoma, also known as low-tension glaucoma, results when your eye pressure doesn’t change or remains normal for you, but somehow, your optic nerve has become damaged. As with other types, there is no known definitive cause for this type of glaucoma.
- Angle-closure glaucoma, also known as closed-angle glaucoma or narrow-angle glaucoma, can be either chronic or acute. This form of the disease is the least common and presents symptoms that include headaches, eye pains, nausea and vomiting, blurred vision, halos, and eye redness that appear before an attack of angle-closure glaucoma. This occurs when the angle between your iris and cornea closes, whether gradually from age or abruptly, which can happen if you already have a narrow opening. The fluid can build rapidly and pressure shoots up as that opening is snapped shut, causing blindness.
- Congenital glaucoma is glaucoma occurring in children, whether from birth or at a very early age. This usually happens from a physical defect in the eye that doesn’t allow it to function normally, but it can also come from some other medical issue.
- Secondary glaucoma comes about when you have another medical or eye issue, and glaucoma follows as a result. Some diagnoses that can lead to secondary glaucoma include tumors, eye injury, inflammation of the eye, diabetes, and certain medications, especially ones that contain steroids.
- Pigmentary glaucoma, or pigment dispersion, blocks the drain of your eye with tiny granules of the eye’s pigment, or the iris, after circulating through the fluid at the front of your eye.
Risk Factors for Glaucoma
A glaucoma suspect is someone who has at least one of the risk factors for glaucoma, but doesn’t have an actual glaucoma diagnosis yet. If you are labeled a glaucoma suspect, your ophthalmologist or New York optometrist may want to see you more frequently to keep a close watch on your eye health and pressure.
Your ophthalmologist more than likely labels you as a glaucoma suspect if you fall into one or more of the following categories:
- You are over 40 years old.
- You have a family history of glaucoma.
- You are of African, Hispanic or Asian heritage.
- You already have high eye pressure.
- You are farsighted or nearsighted.
- You’ve had an eye injury in the past.
- Your corneas are thinner than normal.
- You’ve been diagnosed with diabetes, migraines, hypertension or poor circulation.
If you are having any abnormal visual symptoms, you should always be evaluated with a thorough consultation and examination by a physician for an accurate diagnosis and treatment plan as it may be a symptom or sign of a serious illness or condition.
Few if Any Treatments Available
Unfortunately, glaucoma damage is permanent, which is why it’s so important to get regular eye test, especially if you have any of the risk factors described above. Once you’ve been assigned a glaucoma diagnosis, your NYC doctor’s able to treat you with eye drops that can either decrease your eye fluid production or help to open up the drainage area in your eye.
Your only other option, if your ophthalmologist or New York optometrist decides it’s necessary, is surgery. There are several kinds, depending on what your eye doctor sees as the cause of your glaucoma. You should discuss all of your treatment options with your eye doctor in detail. Your eye care doctor may also ask to see you more frequently, about every three to six months, depending on all of your factors.
Important Reminder: This information is only intended to provide guidance, not a definitive medical advice. Please consult eye doctor about your specific condition. Only a trained, experienced board certified eye doctor can determine an accurate diagnosis and proper treatment.
Do you have any questions about glaucoma treatment in NYC? Would you like to schedule an appointment with NYC ophthalmology doctor Dr. Richard L. Deluca or optometrist Dr. Saba Khodadadian of Manhattan Eye Doctors & Specialists? Please contact our office for consultation with NYC glaucoma specialist and eye doctor.
Dr. Saba Khodadadian, Optometrist (NYC Eye Doctor)
New York, NY 10028
(Between Madison Ave & Park Ave)
☎ (212) 533-4821


